I had a phenomenal ski trip with Jacob, Paul, and Cliff in the Dolomites, using my base Ikon Pass (5 days) to explore Dolomiti Superski over MLK week. This post captures what I did, what I’d do differently, and the notes I’ll want next time. Hopefully you find it useful too. I’ll keep it brief.
Sat, Jan 17 - Land in Venice
We landed in Venice at 4:55pm from Seattle via London. I grabbed 150 euros at the airport.
I activated my Airalo SIM (code: RAJA8345 for a $3 off discount). I made sure to get the Italy one (rather than all of Europe, since that didn’t work well last time).
Our ski bags were delayed by a day, probably because of a tight connection at Heathrow. We got a crash course in Italian inefficiency trying to figure out where everything was. My AirTag showed my ski bag still in London, but the agent at the counter insisted it was on the next flight that night.
Fortunately, we booked lodging nearby for a fantastic rate, so driving back the next morning wasn’t an issue. Jacob had a steep Avis discount through work, so we grabbed a cargo van with plenty of room for the missing gear.
Dinner was at Al Quadrante, one of the only options nearby, and it was genuinely good.
Sun, Jan 18 - Drive to the Dolomites
We walked to breakfast at PanCaffè da Ely, and the boys tried the classic: cornetti, caffè, and spremute (fresh-squeezed OJ). It was high season for Sicilian red oranges, which I only learned after wondering why my spremuta tasted so much better than when I was last here in August.
We drove back to the airport and, after another round of bureaucracy, walked out with our ski gear.
The drive to the Dolomites is a lot more reasonable from Venice than from Milan (2.5hrs vs 3.5hrs). Still, I had us stop in Belluno to break it up. The town is framed by snowy peaks, but a terrain map makes it obvious you’re still in the foothills.
We grabbed essentials at Lidl (house snacks, body wash, lotion, shampoo). I’ve learned over many Airbnb stays in Italy/France not to expect certain items. Lunch was fantastic pizza at Osteria del Tiziano.
We wandered around looking for gelato, only to find the shop was closed until spring, our first of many reminders that Google Maps hours are unreliable. Still, it ended up being a worthwhile walk to soak in the architecture and quiet, narrow streets.
We got back on the road and reached Fontanazzo for the week mid-afternoon, with the cliff faces getting steeper by the kilometer.
Lodging was another unbelievable deal, coming in at under $60 per person each night. We were at most seven minutes from a new gondola (Funivia Campitello - Col Rodella), with a ski bus stop across the street if we wanted it.
For dinner, we parked our large van in Canazei, a far more popular town with more shops and restaurants. Parking was never that hard, but it helps to navigate to a central lot instead of the restaurant address.
For 6:30pm on a Sunday, we got turned away a few times before landing a table at Cianel.
Mon, Jan 19 - Sellaronda CW + Marmolada
We grabbed breakfast at 8am in Campitello di Fassa, then drove higher to the big, empty lot near Hotel Lupe Bianco at the base of the Pradel-Rodella gondola. Pro move: no lift lines at 8:45am, and we were already on the Sellaronda loop, which made navigating the return easy.
Before any skiing, you’re required to buy insurance, which we hoped to do in person. Apparently you can only do it online, according to the person in the booth by the road. She did give us some chocolate to start the day. We completed the process on the gondola ride up from our phones. Also worth noting: your Ikon Pass works on the scanners, no need to get a special Dolomiti pass.
You’re certain to have a great cell signal on any lift or run, by the way. I’d also suggest live-location sharing if you’re with friends. We even used walkie-talkies, which felt like overkill, but they actually saved time.
Unless you’re a bad skier, you shouldn’t have trouble completing the Sellaronda loop in less than five hours, including photo stops, leisurely lunches, and lift lines. Of course, this changes if you start around 9:30am or later (like most people), if you start off the Sellaronda loop, or if you somehow miss the very obvious signs indicating clockwise (orange) and counter-clockwise (green).
We opted to do the CW loop. There was less traversing, and from mountain biking the loop a few months ago, it felt less arbitrary.
We made the smart decision to have an early lunch at 10:20am at the Danterciepes restaurant. It’s one of my favorites: modern, great views, and it won’t break the bank. Having an early lunch meant that we’d have emptier lift lines around noon when everyone else would be eating.
You’d think from all the Reddit posts that lift line etiquette is abysmal in the Dolomites: people stepping on your skis, elbowing you, shoving past you to take the empty space without acknowledging you at all. We were prepared for chaos, but it felt wildly overstated. While there aren’t any orderly lines or lifties directing traffic the way you’d expect in American ski resorts, the European system made perfect sense. People generally filled gaps respectfully. Occasionally you’ll have to edge in to stay with your crew, but it’s not personal.
Despite a below-average snowpack for the Dolomites when we went (less than 50% of average), the snow-making here is world-class. More snow wouldn’t have made a difference on the groomers (every run is groomed). What we really missed was fresh snow covering the brown grass beyond the groomers. A few of the guys opted to bring touring gear in case we went off-piste, but they were a little too optimistic.
Reddit isn’t wrong about one thing: the average skier here is a bad skier. You’ll see a lot of randomly stopping in blind lips.
Our second break was at the Luigi Gorza rifugio, my second favorite place to eat on the loop. It’s another modern structure with an incredible panoramic view.
Cliff had the idea to add on a detour to the Sellaronda by taking lifts and runs over to the top of the Marmolada glacier. The view from 10,500ft is incredible, and absolutely worth it. Skiing down the narrow-ish slope wasn’t my idea of fun, but the boys loved it. I was on my Icelantic 101s, which are not exactly ideal on icy, steep pitches.
In total, our 30mi skiing, 29,900ft descent Sellaronda CW + Marmolada day took us 7hrs with leisurely stops.
We grabbed dinner at Osteria da Besic, making a WhatsApp reservation an hour before they opened.
Tues, Jan 20 - Seceda slopes
We grabbed breakfast in Campitello di Fassa. Despite being a lot smaller, or perhaps because of it, I preferred it much more than the larger Canazei. Bar Pasticceria Marlene would end up being our favorite pasticceria by far. Charming and decked out in old wood, with a raging wood stove in the corner, we had no regrets about lingering and not making first lifts.
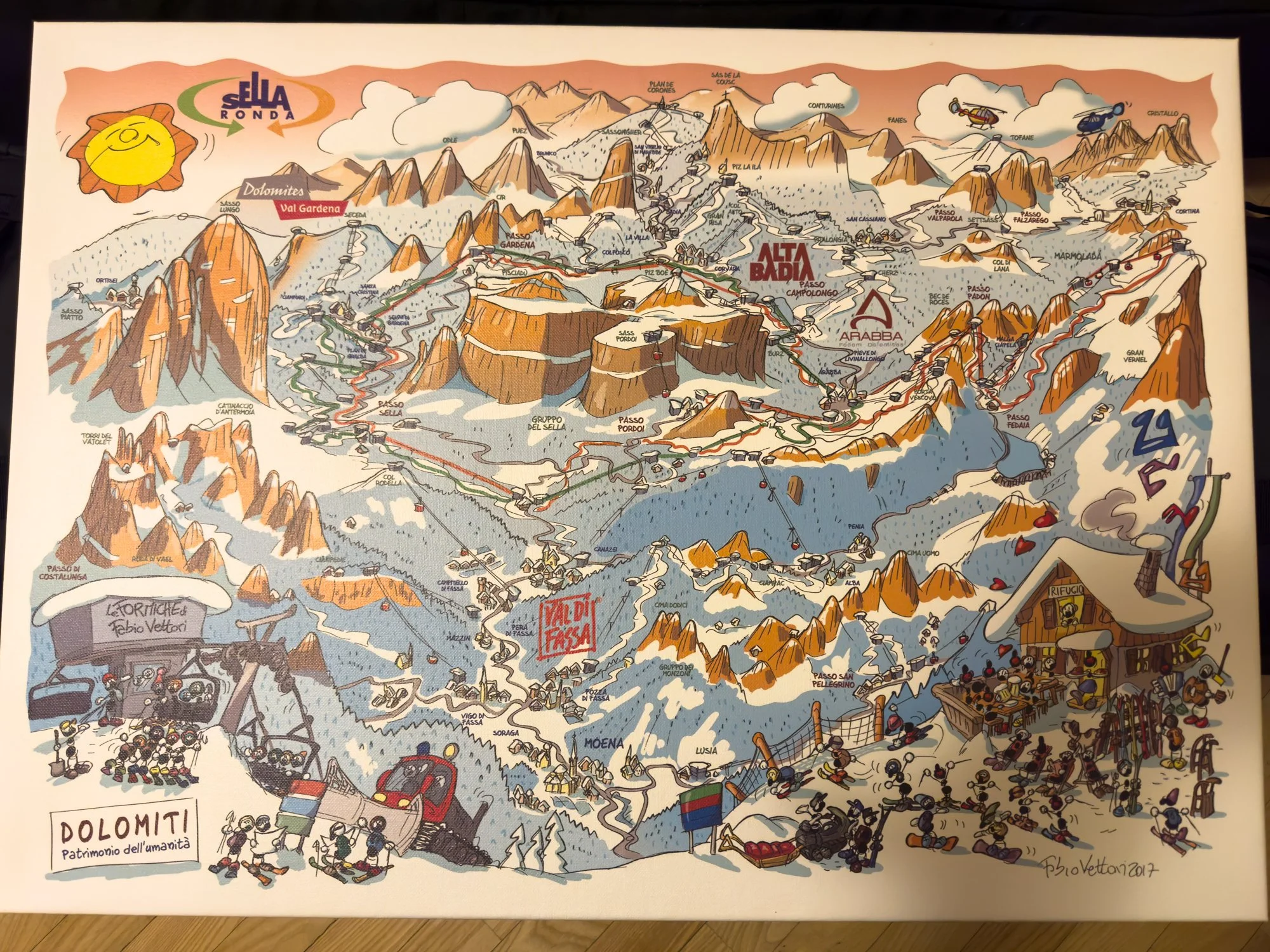
The Sellaronda loop, which goes around the Sella massif, crosses through four main zones (in clockwise order): Val di Fassa, Val Gardena, Alta Badia, and Arabba. Since we’d be starting in the southwest corner on a map, we’d start in Val di Fassa every morning. Today’s plan would be to explore the Seceda ridgeline, accessible by taking a short underground tram (Val Gardena Rhonda Express) within the Val Gardena network.
Seceda takes a bit of logistics, but it’s absolutely worth it. The runs are south-facing, sunny, wide, and give you a constant view of the Sella massif while you descend. When you make it to the top of the lifts, pop your skis off and walk up the small incline (with your skis) to peer over the jagged ridgeline. It’s worth the two-minute detour.
We had lunch at Baita Sofie Hütte, pricier than eating lower down on the Seceda runs thanks to the view.
The Seceda runs were by far my favorite, and it’s an easy way to accumulate a lot of laps if you’re chasing vert. We reversed our journey and made our way back to the core of Val Gardena, ultimately following the Sellaronda CCW (green) signs.
We stopped by Rifugio Salei, where my former Airbnb host and now friend Tommaso was working. He treated the guys each to a bombardino (hot Italian winter cocktail of egg liqueur and brandy, topped with whipped cream and cinnamon or cocoa powder) and gave me a quick tour of the fancy lodge and restaurant.
Cliff was excited to see the sunset at 5pm, so we settled in for a few minutes at Rifugio Des Alpes. The plan was that we’d ski all the way down to our car in the fading twilight. We soon learned that it’s forbidden to be on the slopes after 4:45pm, and we’d need to make it down to Campitello di Fassa via the cable car.
This was a problem because we were parked in nearly the opposite direction, up toward the pass. I had a work call to join at 6pm, so I split off and walked with my ski gear to a bus stop (which was harder to find than I thought). Although I bought a ticket via an app, it was still very confusing how to validate the ticket; the bus driver gave up on me and let me stay on for the one stop. The guys called a local taxi, which cost 40 euros.
Our lodging was just steps away from Pizzeria Lo Scoiattolo, where we had good pizza.
Wed, Jan 21 - More Seceda slopes
We started the next morning again at our favorite cafe, Bar Pasticceria Marlene, indulging in whatever pastry looked good.
Cliff and Paul decided to swap their wide skis at Euroski for skinny groomer skis to rip down with more confidence, after hearing Jacob describe the experience. As the worst skier in the group, I considered it. I fell three times, all because of flat-light iciness. The majestic cliffs jutting up into the sky also have the effect of shading certain aspects of the ski runs, so it can get pretty bulletproof (and cold) at times.
We had plans to drive to Ortisei to get more laps in the Val Garden area. We soon regretted this decision after seeing how long it would take for us to drive there. It would’ve been faster to park in our usual spot and make our way there with skis and lifts. We quickly did paid parking at Plan de Gralba. We worked our way north, eventually cutting west down the very long La Longia run. This ended up being a mistake because we found ourselves in a 30-40 min Seceda Furnes cable car line. We decided not to push further into Ortisei and instead ran laps on Seceda again before making our way back towards the car.
Thur, Jan 22 - Solo start to Alta Badia
Cliff and Paul wanted to maximize their vert so they set off early. I waited with Jacob while he got his gear adjusted at the boot fitter in town. I wasn’t in a rush. My morale was a bit low from having fallen earlier.
I set off solo, opting into the Sellaronda again but peeling off halfway to spend focused time in Alta Badia. It had a reputation of being sunnier and mellower, and I was curious to get a view of the Sella massif from that angle.
The runs were either short and mellow or long and flat. There were more couples and families, and the off-piste coverage was noticeably thinner. I didn’t mind. I was really on a sightseeing tour with this trip.
I did end up running into Paul and Cliff, who had gone all the way out to Lagazuoi (Hidden Valley). More on that later. We paired up for our final laps. Cliff dropped his goal of trying out the Marmolada glacier with his new rentals after he had a collision with a fence on a bridge crossing.
I was happy to have a buddy to go up the Sass Pordoi cable car with me. We left our skis at the bottom of the cable car and went up for some views. On a heavier snow year, there’s some fantastic touring at the top of the Sella massif. Instead, we soaked in the views, and I had one of the best hot chocolates I’ve ever tasted.
Fri, Jan 23 - Sellaronda + Cortina
Cliff proposed that we try to make our way all the way to Cortina. Given where we were based, it’d mean doing a full loop of the Sellaronda, taking a ski shuttle bus and even a horse-drawn rope tow in addition to all the gondolas and lifts. My buddy Tommaso said it was probably too ambitious. If we weren’t on top of our game, we’d be paying for a very expensive taxi ride back.
I was feeling more confident in my skiing, familiar enough now with the terrain that I could spot icy sections from afar and burn off speed before getting burned myself.
That morning, we ate leftovers and snack bars for breakfast in the parking lot before the first gondola took off, instead of having our usual Italian breakfast of champions. The day started off overcast, but the clouds were just high enough that we had some views.
Cliff was doing his best to keep us hustling. He reluctantly allowed Jacob to grab a cornetto to-go from a takeout window at the top of a gondola. We split up across chairlifts when necessary, edged our way through crowds at the bottom, and tore down the slopes. We were making excellent time and made it to the bottom of the Almentarola run and clicked out of our skis at 10:30am.
Next was a shuttle bus from near Hotel Almentarola to Passo Falzarego for 8 euros per person. I was grateful to have gotten cash at the airport earlier. The bus doesn’t leave until it mostly fills up, which didn’t take very long. The drive itself took a little over ten minutes and you’d think the bus driver was inspired by F1 racing by the line he took on the curvy mountain road. He even had a timer above his head which we joked was how he tracked his personal bests.
Once we got dropped off, we walked with our skis a short distance and did a somewhat lengthy traverse on thin-cover snow to the Skyline Cortina gondola. It’s a scenic ~3-mile gondola that drops you right onto the Cortina side.
If the snow was thin in Alta Badia, it was even thinner here further east in Cortina. We stopped for lunch at Rifugio Socrepes before weaving our way to the gondola that would take us to the very top.
Cortina would be hosting the Winter Olympics in two weeks, and we were pretty sure we saw some Olympic level athletes working the slopes. Cortina had both extremes: steep and long slopes, as well as short and mellow slopes. The one thing they had in common was the abundant sunshine and the incredible views. We all agreed that the views here were consistently more aesthetically pleasing than the Sellaronda.
We made a few wrong turns and were getting antsy about missing our self-imposed cutoff time of being back on the Skyline gondola by 1pm. Deciding to ski from the top was already pushing it. We made it back to the Skyline gondola seven minutes later than we wanted, and then we were locked in. No more stops until we were back on the Sellaronda.
Getting back to the Sellaronda would be one of the more memorable aspects of the entire trip. There was an incredible amount of flat traversing, requiring skate skiing skills that I was weak on. If you’re a snowboarder, don’t even think about it. We also had some of the most beautiful chairlift rides I’ve ever had, and we got to ski Lagazuoi, known as the hidden valley. My only regret from the entire trip is that I had to admire the views while hurtling past other skiers at speed. I wish I could’ve stopped for a photo. The photo you see is from Cliff the day before.
If that wasn’t memorable enough, when we returned to the valley floor, we got on a horse-drawn rope tow. For 5 euros per person, we were pulled along the mostly-flat path. If you don’t have cash, you’ll have to skate ski the way back to Almentarola (which isn’t too bad).
We made our way back to the Sellaronda CW loop and knew we were in the clear. We didn’t have time to spare though. Unfortunately, Cliff had two more collisions: one with a reckless Brit going too fast and another one minutes later on the steep, shaded, and crowded bumpy runs of Arabba in the afternoon (everyone’s least favorite section of the Sellaronda).
We got back to the car with only minutes to spare. We had covered 80 miles of terrain (46mi on skis) and done 36,600 feet of descent on our final day. We treated ourselves to a fantastic dinner at La Telia/Italia where they had what I would consider the best pizza of the trip (tartufo is the move).
In the town of Canazei there was a festival of some sort going on. We didn’t stay long enough to figure out what was going on, but many locals were dressed in traditional alpine attire.
Sat, Jan 24 - Evening in Venice
We woke up to fresh snow on the ground. A storm was moving through, and the forecast over the next 24 hours was 8–10 inches. We had a leisurely (and delicious) breakfast at Bar e Snack Zirm. Don’t miss out on their sandwiches; one can be shared easily.
As we made our way south to Venice, we had some small mountain passes to cover. Despite requesting snow tires, we didn’t get them. We assumed we had snow chains, so we pulled onto a wide shoulder to put them on as the van started losing traction on the icy tarmac.
We soon learned that the package that we assumed was snow chains was actually a first aid kit. Over the next hour, we used spotty cell signal to wait on hold, have our calls dropped, and work our way through Italian and English to try and get help. Ultimately, we decided to reverse the van and turn it around, carefully rolling our way down the road back into town. We were forced now to take the long way to Venice, through Trento. That route stayed below the freezing level that day, so it felt safer.
After dropping our stuff at the Airbnb (the same one near the airport), we drove into Venice and parked at the main lot by the train station. I’m not sure if reservations are required during busy season, but we had no issue. The few hours we were there would cost only 15 euros, a bargain compared to taking public transit for four of us.
We speed walked a mile from Piazzale Roma to Ponte Rialto, ultimately ending up at Antica ai Tre Leoni. I made a reservation here via email. The meal was fine and pricier than what we were used to. I wanted to be in that area of the city in the evening, otherwise I’d have chosen a different restaurant.
We had gelato at Suso, which has two locations near each other. Most of the top gelato shops were closed during the off season. We all agreed that Venice was fun to walk through at night, with all the beautiful lighting from ornate windows reflecting off of the damp, polished stones.
We walked through Piazza San Marco before hopping on the Line 1 ferry, which weaves along the Grand Canal back toward the parking lot. The 51-minute ride from S. Marco-San Zaccaria "C" dock cost 9.5 euros per person. There are many kiosks by the docks to buy tickets (you want the 75’ one), but there’s also tap to pay at the gate of the docks.
The ferry ride itself, which we started at 8:40pm, allowed us to see the grand palazzos, arches, churches, and bridges from the water without spending a fortune. We were late enough that we had the stern of the small ferry to ourselves for 80% of the ride.














Sun, Jan 25 - Flight home
It was an uneventful flight back home, focused primarily on typing this up.
Tips for next time
Base yourself near a gondola, not in a “popular” town. Being 5 to 10 minutes from a lift (Campitello for us) mattered more than being walkable to nightlife. Places close early and you’ll save energy every single morning.
Start early on big objective days. Parking at the Pradel–Rodella gondola before 8:45am meant zero lines and an easy Sellaronda return. Anything after ~9:30am adds friction everywhere; you’re just part of the crowd.
Do Sellaronda on Day 1 if possible. It orients you fast. After that, navigating Val Gardena, Alta Badia, and Arabba becomes intuitive.
Clockwise (orange) felt smoother than counter-clockwise. Less traversing, cleaner flow, and easier pacing.
Eat lunch early (10:15 to 10:45am). We had empty lifts while everyone else was eating. Danterciepes and Luigi Gorza were perfect for this.
Seceda is a highligh. Sunny, wide, long laps with nonstop views. Walk the extra two minutes at the top for the ridgeline lookout.
Alta Badia is mellow sightseeing; Arabba gets icy and chaotic late day. Plan your energy accordingly.
Cortina in a single day is ambitious but doable. You need to move with purpose, be comfortable skate skiing long flats, and respect hard cutoff times for gondolas. Snowboarders should probably skip it. Snowboarders should also consider learning to ski, just kidding. Fun fact: 98% of folks on the mountain are on skis.
Carry some cash. Shuttle buses, horse tow, random rifugios, and small cafes still want euros. Get euros at arrival at the airport while you wait for your ski bags.
Buy the required ski insurance online. You cannot reliably do it in person. Takes five minutes on your phone.
Share live location with your group. Cell service is excellent on lifts and runs. This saved us time multiple times.
Expect flat light and bulletproof shade. The towering cliffs cast long shadows. If you’re on wider skis, consider swapping to groomer skis for confidence on icy pitches.
Google Maps hours are unreliable in winter. Especially for gelato and shoulder-season businesses. Have backups.
If you rent a car, confirm winter tires explicitly. Do not assume. Also check that your “snow chains” are actually snow chains.
Venice works surprisingly well as an evening stop. Park at Piazzale Roma, walk to Rialto, then take Line 1 down the Grand Canal after dark. It’s scenic, efficient, and far cheaper than a private boat.
Stay near the Venice airport. Your ski bags can get delayed and it’s super easy to get into Venice for day-tripping.